Throughout medical history, numerous treatments have emerged, hailed as groundbreaking advancements, only to be abandoned years later. While some were initially celebrated for their effectiveness, others fell out of use due to unforeseen side effects or the development of better alternatives. In this article, we’ll explore 14 medical treatments that, despite once being considered revolutionary, eventually faded from practice. From dangerous practices like bloodletting to now-outdated drugs like thalidomide, these treatments offer a glimpse into the ever-evolving nature of medicine. By examining their rise and fall, we can better understand how far we’ve come in the pursuit of safer, more effective care.
Mercury Treatment for Syphilis
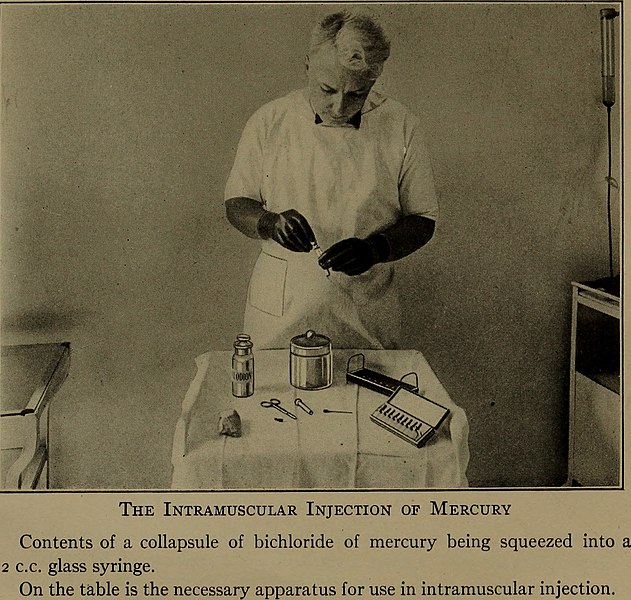
Mercury, once hailed as a miraculous cure for syphilis, was widely used from the 16th century until the early 20th century. Physicians believed mercury’s toxic properties could combat the bacteria causing the disease. However, prolonged mercury exposure led to severe side effects, including organ damage, tremors, and death. As new, more effective antibiotics like penicillin emerged in the mid-20th century, mercury quickly fell out of favor. Researchers found that penicillin offered a safer and more targeted treatment without the toxic risks. Despite its historical significance, mercury treatment is now viewed as a dangerous and outdated practice. Modern syphilis treatments have come a long way, with antibiotics taking the lead.
Lobotomy

The lobotomy, developed in the 1930s, was once considered a revolutionary treatment for mental health conditions such as schizophrenia and depression. By severing connections in the brain’s frontal lobes, doctors hoped to relieve patients of debilitating symptoms. Initially, many patients showed signs of improvement, but the procedure often led to severe cognitive deficits and personality changes. Over time, the negative effects outweighed the benefits, and new antipsychotic medications like Thorazine emerged. The lobotomy quickly fell out of favor as the psychiatric community moved toward more humane and effective treatments. Today, it is seen as a horrific and unethical chapter in medical history. Neurosurgery for mental health disorders has since evolved, focusing on more precise techniques with far less risk.
Radium Therapy
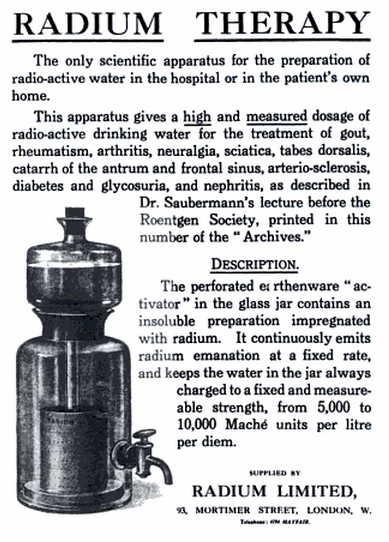
Radium, discovered in the early 20th century, was once hailed as a miracle cure for a variety of ailments, including cancer. Its radioactive properties were thought to help shrink tumors and relieve pain, and radium was used in treatments ranging from cancer therapy to promoting general health. However, over time, it became clear that exposure to radium led to severe radiation poisoning and cancers, especially bone cancer. By the mid-20th century, safer alternatives like chemotherapy and radiation therapy emerged, rendering radium therapy obsolete. Modern cancer treatments are far more targeted and less harmful than those based on radiation exposure. Despite its dangerous legacy, radium therapy remains a pivotal lesson in the development of safe medical practices. Its fall from use marked a significant shift in cancer treatment.
Bloodletting

One of the oldest medical treatments, bloodletting, was practiced for thousands of years as a cure for various conditions, including fever, headaches, and infections. The idea was rooted in the belief that imbalances in the body’s four humors (blood, phlegm, yellow bile, and black bile) caused illness. By draining blood from a patient, doctors believed they could restore balance and promote healing. However, as medical science advanced, bloodletting was shown to often worsen conditions by depleting the body’s vital resources. The development of antibiotics and a better understanding of disease transmission gradually replaced bloodletting with more effective treatments. Today, the practice is seen as archaic and harmful, yet it was once widely accepted by physicians. It remains a reminder of how far medicine has come in understanding human health.
Thalidomide
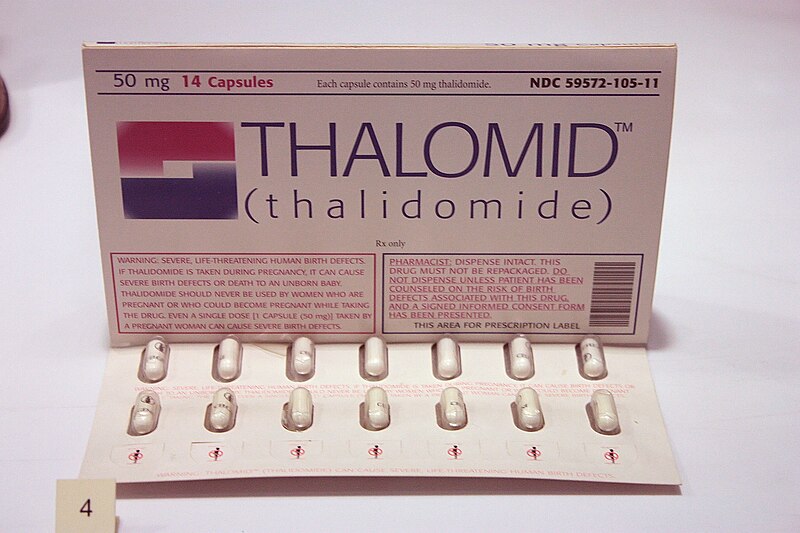
Thalidomide, first marketed in the 1950s as a treatment for insomnia and nausea during pregnancy, was hailed as a safe and mild sedative. Unfortunately, it was later discovered that the drug caused severe birth defects, leading to thousands of children being born with malformed limbs. This tragic outcome led to its withdrawal from the market, but thalidomide was eventually rediscovered as a treatment for conditions like multiple myeloma and leprosy. Despite its return to use for specific ailments, the drug’s reputation was permanently tarnished. The thalidomide tragedy played a crucial role in shaping modern drug approval processes, leading to stricter regulations and safety standards. Today, thalidomide is used under strict supervision, but its history serves as a somber reminder of the potential dangers of new drugs. The case is an example of how medical breakthroughs can be both promising and perilous.
Mummy Powder

In medieval and Renaissance Europe, powdered mummies were believed to have healing powers and were used to treat everything from bruises to seizures. The idea came from the belief that mummies contained potent medicinal properties, possibly due to their preservation through embalming. The powdered remains of ancient Egyptian mummies were ground into a fine powder and mixed with other substances for various concoctions. However, the practice eventually fell out of favor as the scientific community recognized the practice was based on superstition rather than evidence. Further investigation into the healing properties of such powders found that they were no more effective than ordinary medicine. Modern archaeology also condemned the practice for contributing to the destruction of valuable cultural artifacts. Today, mummies are respected for their historical significance, not for their supposed medicinal properties.
Insulin Shock Therapy

Insulin shock therapy, or insulin coma therapy, was developed in the 1930s as a treatment for schizophrenia and other mental illnesses. The method involved administering high doses of insulin to induce a coma, under the belief that it would reset the brain’s metabolism and improve psychiatric symptoms. While some patients showed temporary improvement, the therapy was extremely dangerous and often led to severe brain damage, seizures, and even death. By the 1950s, the development of antipsychotic drugs like chlorpromazine offered safer and more effective treatment options. Insulin shock therapy was phased out, and today it is rarely mentioned outside historical discussions of mental health care. The treatment remains a controversial chapter in psychiatric history, illustrating the dangers of early psychiatric interventions. It was a part of a broader shift toward more humane, scientifically supported treatments.
Bovine Serum for Immunization
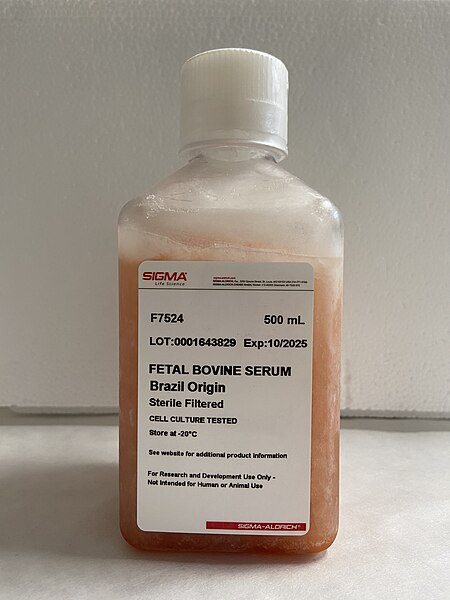
Bovine serum, which comes from cows, was once used as a source of antibodies for immunization, especially during the early 20th century. It was used to treat diseases like diphtheria and tetanus by providing passive immunity to patients. The serum was thought to enhance the body’s immune response, but it often caused allergic reactions and sometimes severe anaphylactic shock. With the discovery of more precise vaccines and improved immunization methods, the use of bovine serum was discontinued. It was later replaced by purified human-derived immunoglobulins and synthetic treatments that were much safer. Today, immunization techniques are based on well-researched vaccines that provide longer-lasting protection without the risks of bovine serum. The shift to safer and more reliable treatments marked a milestone in the history of vaccination.
X-Ray Therapy

In the early 20th century, X-ray therapy was heralded as a miracle treatment for a variety of conditions, from cancer to acne. The technology allowed for targeted radiation to destroy cancer cells or shrink tumors, and it was even used to treat warts and other skin conditions. However, it soon became apparent that excessive exposure to X-rays could cause burns, radiation sickness, and an increased risk of developing new cancers. The therapeutic use of X-rays eventually became obsolete as safer and more effective treatments, like chemotherapy and radiation therapy, were developed. X-ray therapy was also largely replaced by more controlled methods of radiation therapy that limit exposure. Despite its initial success, X-ray therapy’s dangerous side effects and long-term risks led to its discontinuation. It now serves as an important chapter in the history of medical radiation and the evolution of cancer treatment.
Cauterization

Cauterization, the process of burning tissue to treat wounds or stop bleeding, was once a common practice in surgeries. By using a heated instrument, surgeons believed they could seal blood vessels and prevent infection. Despite its widespread use, cauterization often led to severe pain, infection, and long recovery times. The advent of antiseptics and more refined surgical techniques made cauterization obsolete. Today, more precise methods like laser surgery and cauterization using electrical currents have replaced the traditional heat-based method. Although it is still used in certain medical procedures, the painful and dangerous aspects of cauterization have largely been eliminated. Cauterization’s decline reflects the overall progress in surgical techniques, with a focus on reducing patient trauma.
Cocaine as a Local Anesthetic

In the late 19th century, cocaine was introduced as the first local anesthetic and quickly gained popularity among surgeons. Its powerful numbing effects made it highly effective in procedures involving the eyes, ears, and throat. Doctors hailed its ability to block pain, offering patients much-needed relief during surgeries. However, as its addictive properties became more apparent, cocaine’s use in medicine started to decline. Physicians also noticed that prolonged use could cause severe side effects such as convulsions, heart palpitations, and even death. With the advent of safer alternatives like Novocain, which was introduced in the 1900s, cocaine lost its place in medical practice. Today, cocaine is banned in most medical applications due to its high potential for abuse and the availability of more effective anesthetics.
Dinitrophenol (DNP) for Weight Loss

Dinitrophenol, or DNP, was once touted as a miracle weight loss drug in the 1930s. It worked by increasing metabolism and body temperature, causing the body to burn fat at an accelerated rate. While it did lead to rapid weight loss, the drug came with dangerous side effects, including hyperthermia, organ damage, and even death. The medical community quickly recognized the risks associated with DNP and banned its use for weight loss in the 1930s. Despite this, DNP has occasionally resurfaced in underground weight loss circles due to its effectiveness. However, its continued association with fatalities has led to widespread condemnation by health authorities. Today, DNP is considered extremely hazardous and is illegal for use in weight loss treatments.
Snake Oil
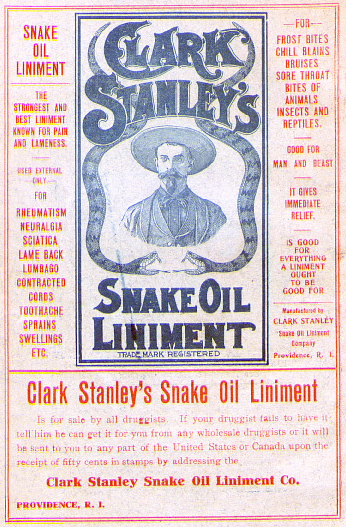
Snake oil was initially marketed as a cure-all remedy in the 19th century, with claims that it could treat ailments ranging from arthritis to hair loss. Made from the oil of snakes, especially the Chinese water snake, it was said to contain healing properties, including anti-inflammatory and analgesic effects. As it gained popularity, snake oil peddlers in the U.S. began adding various ingredients to the product, often without any scientific basis. The use of snake oil as a cure-all was eventually exposed as a hoax, with many brands offering nothing more than a placebo or harmful substances. The term “snake oil” became synonymous with fraudulent or ineffective treatments. Today, it serves as a metaphor for dubious medical practices and scams. Despite its historical popularity, snake oil remains a cautionary tale in the history of medical pseudoscience.
Surgical Removal of the Appendix (Appendectomy) for Non-Acute Appendicitis
Appendectomy, the surgical removal of the appendix, was once routinely performed for all cases of suspected appendicitis, even in non-acute instances. Early in the 20th century, doctors believed that any inflammation of the appendix was a medical emergency that warranted immediate surgery. However, as medical knowledge advanced, it was discovered that not all cases of appendicitis required surgical intervention, particularly in patients with mild or early-stage symptoms. The practice became increasingly scrutinized as better diagnostic tools, such as ultrasounds and CT scans, allowed for more accurate diagnoses. Today, appendectomy is only performed for acute appendicitis, and conservative management is often preferred for less severe cases. The overuse of appendectomy is now considered an outdated and excessive medical practice. As a result, surgery for non-acute appendicitis has largely fallen out of favor.
This article originally appeared on Rarest.org.
More From Rarest.Org
Collecting vintage scientific instruments isn’t just a hobby; it’s a journey into history and innovation. They embody centuries-old craftsmanship, scientific discovery, and timeless elegance. Read more.
Video game consoles have come and gone over the years, with some fading into obscurity while others became iconic. However, not every system that hit the market left a lasting impression. From ambitious hardware to unique concepts, many classic consoles vanished due to poor sales, limited game libraries, or fierce competition. Read more.
Throughout history, people across civilizations crafted drinks that did more than just quench thirst, they brought people together. Some of the world’s oldest alcoholic beverages reveal a deep connection to culture, ritual, and community. Read more.



